Inadvertent hypothermia is considered one of the number one complications of anesthesia, trauma, and some illnesses. When considering potential complications of an illness or anesthetic procedure, the significance of hypothermia is often underappreciated. In addition, the management of hypothermia is not without its own potential risks. Avoidance of inadvertent injury requires both persistent monitoring and due diligence in understanding the currently available warming methods, as well as their benefits and risks. Below is a brief review on hypothermia, the importance of thermoregulation, and risk factors to consider when providing patient warming.
What is Hypothermia?
A condition that occurs when core body temperature drops below what is physiologically normal for that species. Normal core temperature varies significantly between species. Core temperature is tightly regulated, and the thermoregulatory process is quite complex; thus, will not be the scope of this review. Causes of heat loss are often the result of many compounding factors and adverse effects are vast and largely dependent on the degree of heat loss.
Adverse Effects Associated with Hypothermia
Hypothermia, particularly when severe, can result in a significant number of important complications. The severity of these complications directly correlates to the severity of the hypothermia. Some of these complications include slow recovery from anesthesia, myocardial ischemia, arrhythmias, hypotension, decreased response to vasoactive drugs or anticholinergics, coagulopathies, wound infections, and decreased wound healing, just to name a few (VanVeelen 2021, Rauch 2021). These adverse effects not only increase the risk of morbidity and mortality but also can result in longer hospital stays and more costs to your clients.
Mechanisms of Heat Loss
- Evaporation – body moisture containing heat dissipates into the air, pulling heat with it. This can be through the respiratory tract or open wounds/cavities (Sessler 2000).
- Radiation – transfer of heat from the body to objects in the environment, without being in contact with them, via photons and thus are independent of the temperature of the intervening air. This is often the largest contributor to heat loss perioperatively (Sessler 2000).
- Conduction – direct transfer of heat from one surface to a second adjacent surface & is proportional to the difference in the surface temperatures and any insulation between them (e.g. cold table, cage floors, etc.) (Sessler 2000).
- Convection – transfer of heat from the body surface to moving air surrounding the body. The “wind-chill factor”. The second most important source of heat loss during anesthesia and surgery. It becomes the dominant source of heat loss in highly convective environments, such as laminar flow surgical suites (Sessler 2000).
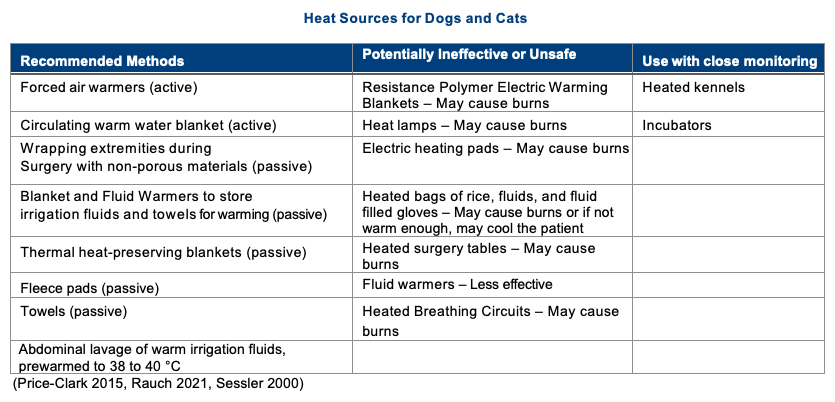
Recommended Methods for Minimizing and/or Managing Hypothermia
Active warming should begin before a patient is anesthetized, in any patient being heavily sedated or undergoing general anesthesia for more than 20 minutes, or sooner in very small patients. This will not prevent but reduce how quickly and to what degree of heat loss occurs. Active techniques for warming are by far more effective than passive techniques, thus passive methods should be used in combination with active methods to be most useful.
Monitoring
Monitoring is a key component in thermoregulation and patient care. Very small patients with large body surface area, those with minimal muscle mass or fat, those undergoing anesthesia, and those having open cavity procedures or that will be wet, as a consequence of the procedure, are prone to becoming hypothermic rapidly. The frequency of monitoring should be based on the individual. Anesthetic patients should have their temperature monitored at least every 15 minutes or more frequently. The frequency for those awake will largely depend on the presenting temperature, mode of rewarming, and other co-morbidity factors (e.g. oxygen dependence).
Summary
Hypothermia is nothing to take lightly. It can have significant consequences and proactive warming should be provided and temperature monitored frequently, to ensure progress and avoid over-heating the patient. There are many devices available. Some of these devices are not only ineffective but may cause more harm than good, thus it is important to do your research before using any device. References used for this article are listed below and can be referenced for a more in-depth review.
References
Price-Clark, S. “Inadvertent Perianesthetic Hypothermia in Small Animal Patients.” Vet Clin Small Animal, Elsevier, 2015, pp 983-994
Rauch, S, Miller, C, Brauer,A, et al. “Perioperative Hypothermia-A Narrative Review.” Int. J. Environ. Res. Public Health, 2021,18,8749. https:// doi.org/10.3390/ijerph18168749
Sessler, DI, Todd, MM (Ed.) “Perioperative Heat Balance.” Anesthesiology, vol. 9, no. 2, 2000, pp. 578-96
VanVeelen, MJ, Maeder, MB. “Hypothermia in Trauma.” Int. J. Environ. Res. Public Health, 2021, 18, 8719. https://doi.org/10.3390/ ijerph18168719



